Loupes Maintenance as a Clinical and Ergonomic Control

ErgoPractice News – Jan/Feb 2026
By Paul Wisniewski, CSSGB
paulw@surgitel.com
Why Routine Inspection, Cleaning/Disinfection, Manufacturer Checkups, and Backup Systems Matter
Summary
Dental and surgical loupes are not just magnification devices; they are clinical tools that impact infection control, visual performance, precision, and clinician posture. As a wearable device used in patient care environments, dental and surgical loupes are exposed to aerosols, spatters, disinfectants, and mechanical stress. Over time, small changes such as scratched optics or lenses, loose hinges, worn nose pads, stretched head straps, and uncorrected prescription changes can subtly impair the visual quality. This natural degradation of the loupe often prompts the clinician to unconsciously compensate by leaning forward, bending the neck, and tensing the shoulders.
This paper outlines the appropriate care and maintenance of dental and surgical loupes:
- Routine inspection and maintenance to preserve fit and optimal performance.
- Proper cleaning and disinfection following contaminated usage (following manufacturer instructions).
- Regular manufacturer checkups, along with replacement of parts.
- Routine prescription updates to maintain working distance and posture.
- A backup loupe to prevent downtime, cancellations, or ergonomic backsliding.
Loupes Live in the Splash Zone: Cleaning, Disinfecting, and IFU Compliance
In dentistry and many clinical environments, loupes and face protection are routinely exposed to contamination during patient care. Although the loupes are not technically “patient contact,” they sit in close proximity to the face and are reused repeatedly, making consistent cleaning and disinfection between patients a sensible and important infection-prevention control. A study on dental loupes found that following manufacturer cleaning instructions can greatly reduce bacterial contamination on the surface,1 yet many clinicians do not disinfect as consistently as recommended. This highlights the need for regular, correct upkeep to reduce cross-contamination risk. The U.S. Centers for Disease Control and Prevention (CDC) recommends that, at minimum, noncritical patient care devices are disinfected when visibly soiled and on a routine schedule, such as after each patient or at regular daily or weekly intervals.2
It is important to follow the manufacturer’s instructions for use (IFUs) and use only compatible, tested products. Manufacturers develop specific protocols for cleaning first, disinfecting second, minimizing excess moisture, and avoiding liquid intrusion into optical assemblies. For example, SurgiTel provides approved cleaning and disinfectant options, and other manufacturers similarly publish disinfection guidelines for loupes and lights. This matters because harsh or incompatible chemicals can degrade lens coatings and plastics over time, reducing clarity and increasing glare; the opposite of what loupes are designed to deliver.
- Clean first, disinfect second, and dry properly.
- Minimize liquid intrusion into optical assemblies.
- Store loupes dry, protected, and away from extreme heat.
Inspection + Maintenance: Tiny Defects Become Big Problems
Loupes are fine-tuned mechanical devices. Hinges loosen, frames drift out of adjustment, coatings degrade, and optics shift out of alignment. The most common trouble spots of a loupe are subtle:
- Lens contamination build-up (film, residue) reducing contrast.
- Micro-scratches increase glare and “haze.”
- Loose hinges/bridge causes vertical or lens decentration.
- Bent frames or shifting nose pads change the alignment of the optics.
- Headband/strap stretch causes sag and alters the declination angle.
It’s not always apparent how much of a problem this creates in the moment. However, over time, this can cause visual strain, decreased performance, and lead to compensatory posture.
Recommended Routine Inspection Schedule
To catch problems early, clinicians can follow a simple routine inspection and maintenance schedule.
- Daily: Wipe down lenses, check for haze or buildup, disinfect frame contact areas per the manufacturer’s IFU, and store loupes in a protective case.
- Weekly: Take five minutes to inspect lens clarity and coatings, confirm hinge tightness, evaluate nose pad wear and head strap tension, and ensure the oculars remain properly aligned.
- Monthly: reassess whether working distance still feels “right” and complete a quick posture self-audit. Are you leaning closer, raising your shoulders, or increasing neck flexion to see clearly?
- After a contamination event: Handle the loupes as soiled eye protection. Use gloves, isolate them appropriately, and clean and disinfect according to the manufacturer’s IFU.
- Annually (or as needed): Vision check and update the prescription or reading power and a manufacturer tune up.
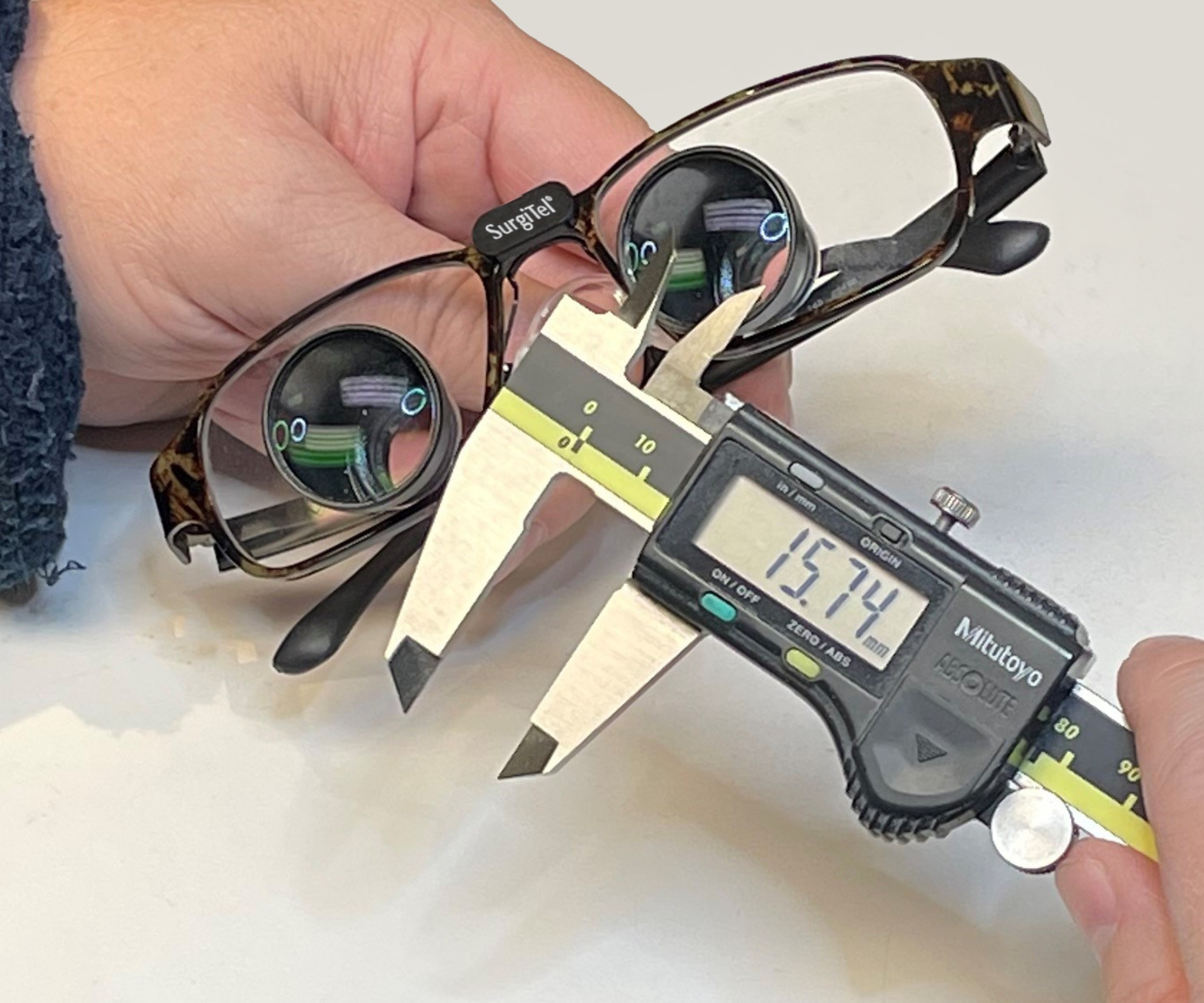
Manufacturer Checkups and Consumables: Treat Loupes as Calibrated Equipment
In a quality mindset, loupes should be treated like any other precision tool. They need periodic assessment to ensure proper optical alignment, a secure frame fit, strong hinge integrity, and component wear.
The small parts matter more than most clinicians realize because they dictate fit and stability, which influences optical performance and, ultimately, posture. Components like nose pads, temple tips, head straps, prescription inserts, and protective lens shields all play a role in keeping everything properly aligned.
Recommended practice: schedule manufacturer checkups or service intervals if you notice recurring fogging or residue buildup, find your posture drifting forward or backwards, experience headaches or eye strain, have a prescription change, or if your loupe has been dropped or impacted.
Prescription Drift: The Hidden Posture Change No One Notices
Changes in vision, particularly after age 40, are common occurrences. Presbyopia is an age-related vision change characterized by a diminished capacity to focus on close objects, which may impact comfort and clarity of vision at working distances.
As vision changes, clinicians may be unknowingly adapting to these changes by:
- Moving closer or further back to see clearly and in focus
- Tilting head/neck position to find a “sweet spot”
- Adjusting shoulders/arms to stabilize
Even small changes can gradually shift posture and increase fatigue.
Best Practices:
- Schedule routine vision exams.
- Update prescription lenses within the ocular/carrier lenses as needed.
- Verify working distance and declination angle, especially when there are prescription changes.
Why Every Clinician Needs a Backup Pair of Loupes
A backup pair is not a luxury, it’s operational resiliency.
The Clinical Reality
When your primary loupe is in for service, damaged, or contaminated beyond immediate use, you face a difficult choice: cancel procedures, work without magnification (often at the expense of posture and precision), or borrow a loupe that may not fit properly or be clean.
Even a backup with lower magnification or a different mounting style will help maintain continuity of care while protecting the clinician’s ergonomics.
TTL vs. FLM as a Backup Strategy
Through-the-Lens (TTL) loupes are typically optimized to your exact working distance, posture, and prescription, making them highly precise but also more dependent on perfect alignment.
Front-Lens-Mounted (FLM) loupes, on the other hand, are more adjustable and adaptable. Features like P.D. adjustment knobs and vertical slides make them a practical backup option, especially if prescription needs or working distance may vary, and they can even be shared between clinicals in a pinch.
Practical recommendation:
- Primary: your best-fit, day-to-day loupe (often TTL)
- Backup: a durable, serviceable alternative (often flip-up or a lower mag TTL) that still supports neutral posture
Conclusion
Loupes are a cornerstone of clinical performance and ergonomic longevity. Proper maintenance of loupes through inspection, correct cleaning and disinfection, manufacturer checkups, timely replacement of parts, and updated prescriptions enable clinicians to maintain clear vision and neutral posture. Evidence supports that magnification systems can improve working posture, but the ergonomic benefit depends on a stable working distance and well-fitted optics.
Finally, clinics and clinicians should treat backup loupes as a standard of care for continuity and ergonomics. A backup pair reduces downtime, protects posture during service events, and supports consistent clinical outcomes.
References
- Zwicker, Denise H., Richard B. Price, Lynzi Carr, and Yung-Hua Li. “Disinfection of Dental Loupes.” The Journal of the American Dental Association 150, no. 8 (August 2019): 689–94. https://doi.org/10.1016/j.adaj.2019.03.008.
- “Recommendations for Disinfection and Sterilization in Healthcare Facilities.” Centers for Disease Control and Prevention. Accessed January 30, 2026. https://www.cdc.gov/infection-control/hcp/disinfection-sterilization/summary-recommendations.html#:~:text=Ensure%20that%2C%20at%20a%20minimum,once%20daily%20or%20once%20weekly).



